Borderline Personality Disorder (BPD), like other mental illnesses, is a brain disease
People with BPD have significant differences in:
Brain Structure
Some parts of the brain exhibit smaller than normal volumes, while other parts of the brain are larger than normal when compared to healthy adults.
Brain Function
Some parts of the brain show greater activity while stimulated, while other parts show reduced activity when compared to healthy adults.
Brain Chemistry
Many people with BPD show disruption and dysregulation of the neurotransmitters which regulate communication between parts of the brain.
Brain components and differences in those with BPD
Amygdala
Description: The amygdala is a key brain structure involved in processing emotions, triggering physiological responses, forming memories, and influencing social and decision-making behaviors.
Differences in those living with BPD:
an increased amygdala
hyper-responsiveness
Exaggerated reactions to perceived threats or social rejection
Impulsive aggression
Emotional dysregulation
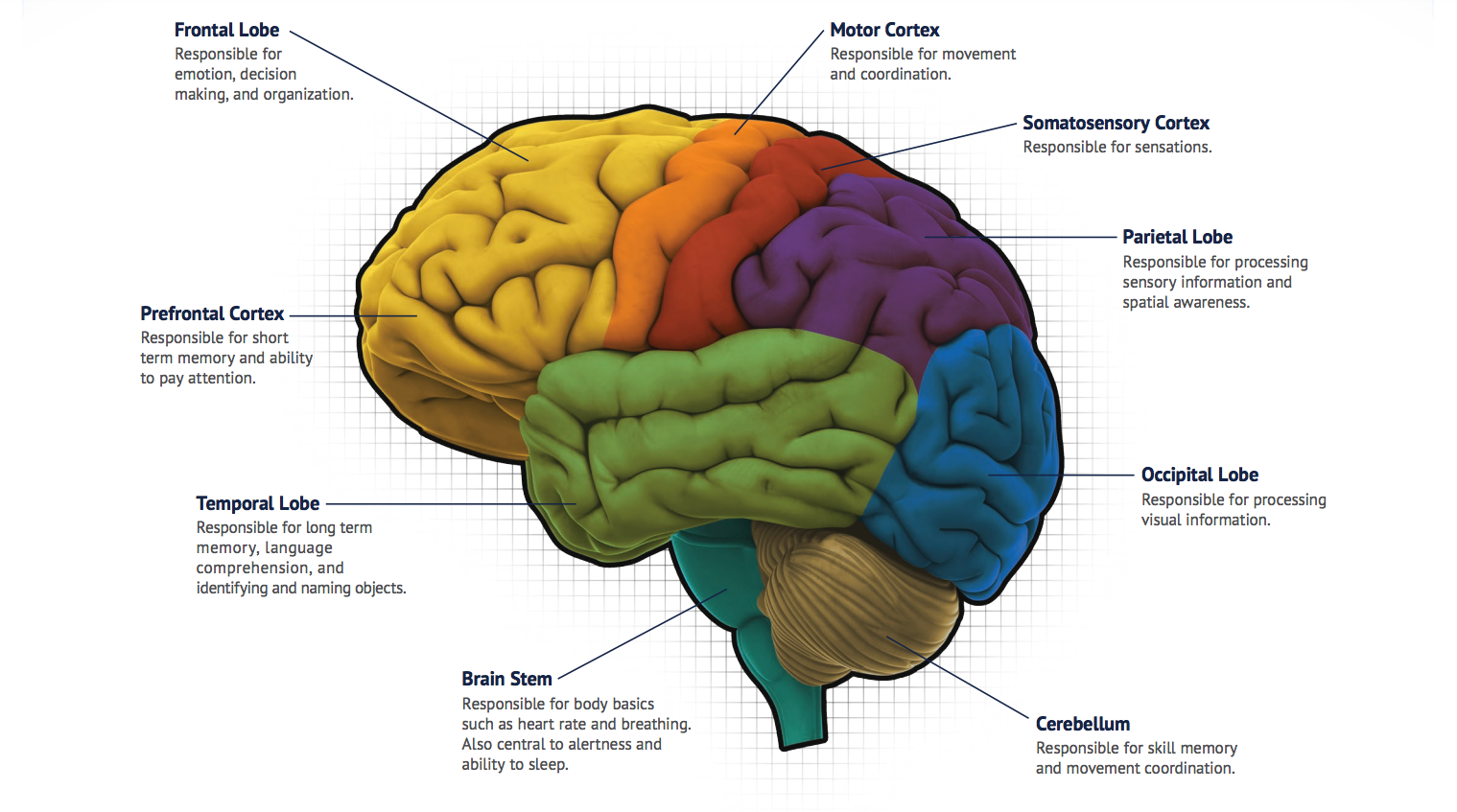
Prefrontal Cortex
Description: The prefrontal cortex is essential for a wide range of cognitive, emotional, and social functions. It enables individuals to plan, organize, make decisions, regulate their emotions, and interact effectively with their environment.
Differences in those living with BPD:
Reduced gray matter volume
Impaired judgement
Emotional instability
Hippocampus
Description: The hippocampus plays a critical role in memory, spatial navigation, and emotional regulation.
Differences in those living with BPD:
Reduced hippocampal volume
Emotional hyperarousal
Intrusive memories
Identity fragmentation
Parietal Cortex
Definition: The parietal cortex is essential for integrating and interpreting sensory information, processing spatial relationships, guiding motor actions, and supporting cognitive functions related to attention, decision-making, and language.
Differences in those living with BPD:
Abnormal parietal activity
Deficits in executive functioning
Problems in planning and organizing space
Neurotransmitters
Serotonin, dopamine, glutamate, oxytocin
Definition: Neurotransmitters are often referred to as the body's chemical messengers. They are the molecules used by the nervous system to transmit messages between neurons, or from neurons to muscles.
Differences in those living with BPD:
Dysregulation of the neurotransmitter systems
Difficulty controlling impulses, aggression, emotional regulation, reward processing difficulties, relational difficulties, chronic dysphoria, self-injury, and suicidality.
Causes of Brain Differences
Genetic Contributions
Family, twin and adoption studies indicate that BPD traits can be inherited. For example, studies of twins have found that identical twins have about an 11 times higher risk of developing BPD than non-identical twins.
Prenatal Adversity
Many studies have found an association between prenatal adverse conditions experienced by the mother and the subsequent diagnosis of BPD in the child. Adverse conditions include prenatal tobacco exposure, medical complications, prenatal maternal traumatic stress, familial conflicts, low social support and partnership problems during pregnancy.
Environmental Risk Factors
Repeated exposure to trauma through adverse childhood experiences (ACE’s) are strongly associated with BPD. Repeated exposure to trauma at times of critical brain development can interfere with normal development of brain structures such as the hippocampus, amygdala and prefrontal cortex. Traumatic disruptions during critical periods of brain neurodevelopment can lead to deficits in self-regulation, attachment, and cognitive processing. About 70% of people with BPD report severe trauma in early life.
Attachment Disruptions
Breakdowns of early attachment relationships with caregivers can disrupt emotional regulation and the way our brain acquires, processes, and understands knowledge and information, encompassing all mental processes such as thinking, learning, remembering, paying attention, and problem-solving. People with BPD often have insecure and disorganized patterns of attachment, which leads to emotional dysregulation and chaotic interpersonal relationships.
References
Giannoulis,E; Nousis, C; Sula, L.-J.; Georgitsi, M.-E.; Malogiannis, I. Understanding the Borderline Brain: A Review of Neurobiological Findings in Borderline Personality Disorder (BPD). Biomedicines 2025, 13,1783. https://doi.org/10.3390/biomedicines13071783
Perrotta, G. Neuroanatomical and functional correlates in borderline personality disorder: A narrative review. Ibrain, 2024 Dec 20;11(1):19-31. doi: 10.1002/ibra.12190. eCollection 2025 Spring.
Schwarze CE, Mobascher A, Pallasch B, Hoppe G, Kurz M, Hellhammer DH, Lieb K. Prenatal adversity: a risk factor in borderline personality disorder? Psychol Med. 2013 Jun;43(6):1279-91. doi: 10.1017/S0033291712002140. Epub 2012 Dec 10. PMID: 23217579.